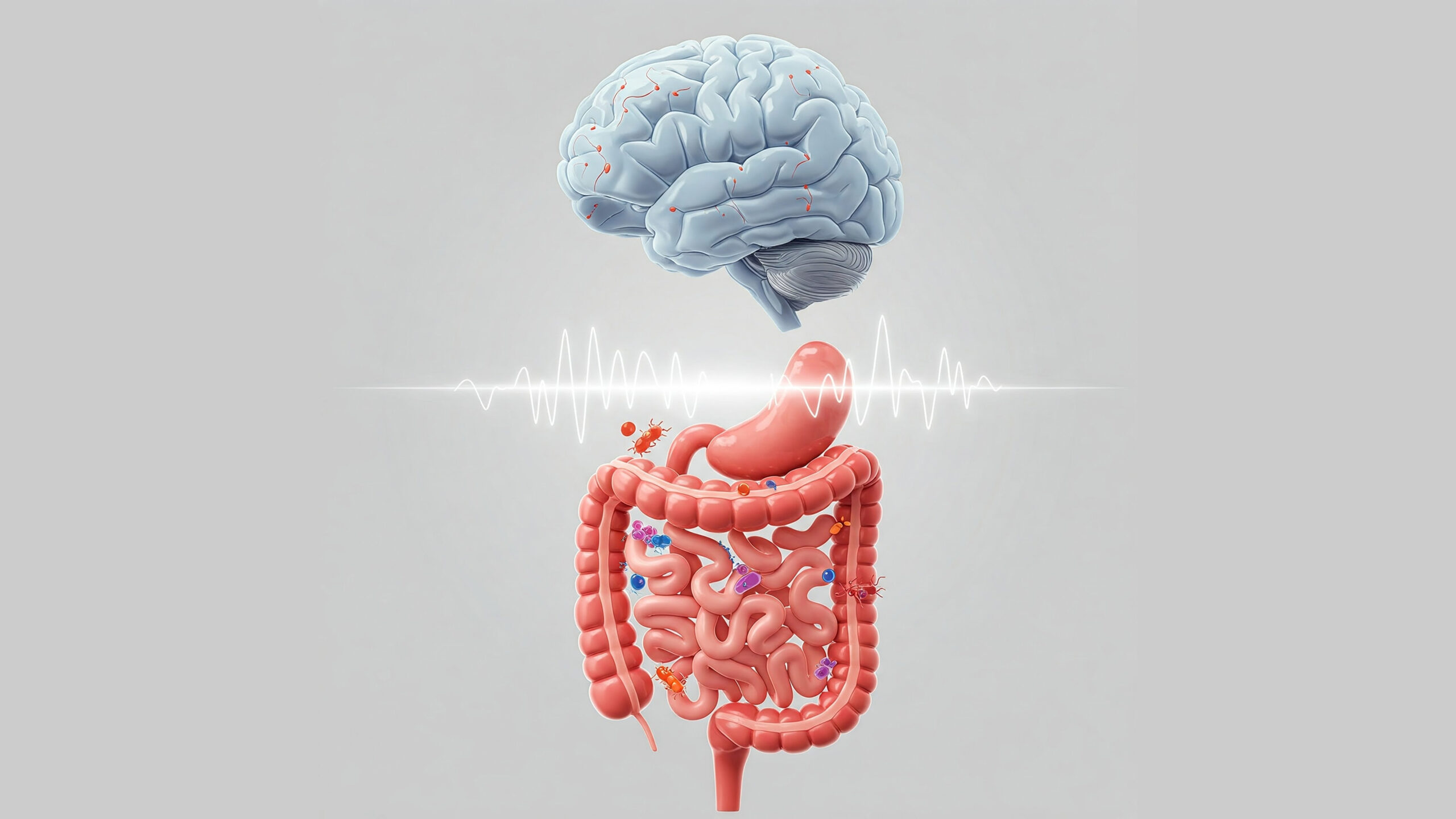
While the pursuit of sharper focus often centers on brain hacks or specific nutrients, the Gut-Brain Axis reveals that true cognitive clarity may start in the gut. This intricate communication network, where the gut—our “second brain”—sends powerful signals to the mind, is deeply influenced by the health of our digestive system. Intermittent Fasting (IF) supports this axis by offering periods of digestive rest, helping rebalance gut microbes, reduce inflammation, and strengthen the gut barrier—factors that can directly impact mental clarity and focus. But IF’s cognitive benefits are amplified when paired with gut-friendly nutrition during eating windows, including fiber, polyphenols, and healthy fats. Together, IF and mindful eating nurture the gut-brain connection, turning digestive health into a key strategy for enhancing concentration, reducing brain fog, and unlocking sustained mental performance.
We often think of the brain as the solitary commander-in-chief, issuing orders from its bony fortress in the skull. But what if I told you there’s another powerful intelligence center deeply involved in how you think, feel, and focus located, surprisingly, in your gut? It sounds a bit strange, but the connection between your digestive system and your brain, known as the Gut-Brain Axis, is a rapidly evolving field of neuroscience, and it holds fascinating implications for anyone using Intermittent Fasting (IF) to achieve better mental clarity. In fact, optimizing this connection might be a key way IF helps sharpen your cognitive function.
Think about those common phrases: “gut feeling,” “butterflies in your stomach,” feeling “sick with worry.” These aren’t just metaphors; they reflect a real, physical communication pathway. Your gut is lined with an intricate network of neurons, sometimes called the “second brain” or Enteric Nervous System (ENS), containing more nerve cells than your spinal cord. This system is in constant dialogue with your main brain via nerves (like the vagus nerve), hormones, and immune system signals [1]. What happens in your gut doesn’t stay in your gut; it sends ripples directly upward, influencing your mood, stress response, and critically, your ability to maintain concentration and think clearly.
So, why bring this up in the context of Intermittent Fasting? Because IF, by its very nature, directly impacts your digestive system. Giving your gut regular breaks from the constant work of digestion isn’t just about resting the physical machinery; it profoundly influences the environment within your gut, including the trillions of microbes residing there – your gut microbiome. These microbes are crucial players in the gut-brain conversation [2]. Changes in their composition or activity, potentially driven by fasting periods, can alter the signals sent to your brain, impacting everything from inflammation levels to neurotransmitter production. Could harnessing the gut-brain axis fasting connection be a hidden key to unlocking sustained focus?
Here we’ll explore the fascinating world of your “second brain,” understand how the gut and brain constantly chat, and examine how Intermittent Fasting acts as a potential modulator of this dialogue. We’ll look at how giving your gut a rest might influence microbial balance, reduce inflammation, and ultimately contribute to clearing brain fog and enhancing cognitive performance. Forget thinking of your stomach as just a food processor; it might be ground zero for boosting your brainpower.
Your “Second Brain”: More Than Just Digestion Down There
Before we link fasting to focus via the gut, let’s appreciate just how sophisticated your digestive system really is. Calling it the “second brain” isn’t just hyperbole; the Enteric Nervous System (ENS) embedded in the walls of your gut is remarkably complex and operates with a surprising degree of autonomy, while also maintaining that critical hotline to your head.
Introducing the Enteric Nervous System (ENS)
Imagine a vast network of neurons – hundreds of millions of them – lining your entire digestive tract, from the esophagus down to the rectum. This network is the ENS [1]. It’s so complex that it can manage the intricate processes of digestion (like muscle contractions, enzyme secretion, blood flow regulation) largely independently, without needing constant input from the brain in your skull. It senses the gut environment, processes information locally, and makes decisions – hence the “second brain” moniker. It uses many of the same neurotransmitters found in the central nervous system, including serotonin, dopamine, and GABA, highlighting its neurological sophistication.
Why is This “Gut Brain” So Important?
The ENS isn’t just coordinating digestion. It plays crucial roles in:
- Nutrient Sensing and Absorption: Detecting the chemical composition of food and regulating absorption.
- Gut Motility: Controlling the rhythmic contractions (peristalsis) that move food along.
- Maintaining the Gut Barrier: Regulating the integrity of the gut lining, which prevents unwanted substances from leaking into the bloodstream.
- Immune Function: Interacting closely with the gut-associated lymphoid tissue (GALT), a major component of your immune system. Roughly 70% of your immune cells reside in the gut!
- Communicating with the CNS: This is where the Gut-Brain Axis comes in – the ENS constantly sends signals up to the brain, influencing mood, stress, and cognition [3].
Your gut is constantly sampling the outside world (via food) and relaying information about it, plus the state of your internal digestive environment, directly to your central command center.
The Gut Microbiome: Trillions of Tiny Influencers
We can’t talk about the gut without mentioning the gut microbiome – the vast community of bacteria, viruses, fungi, and other microbes living primarily in your large intestine [2]. These microbes aren’t just passive passengers; they are metabolically active, producing thousands of compounds that influence both local gut function and systemic health, including brain function. They interact directly with the ENS and the immune system, producing neurotransmitters, short-chain fatty acids (SCFAs), and other molecules that enter the bloodstream or signal via nerves, profoundly impacting the gut-brain axis communication [4]. An imbalance in this microbial community (dysbiosis) is increasingly linked to inflammation, mood disorders, and even cognitive impairment.
Understanding the complexity of the ENS and the influence of the microbiome sets the stage for appreciating how changes induced by intermittent fasting in the gut environment could have far-reaching effects on your mental clarity and focus.
The Gut-Brain Superhighway: How Your Stomach Talks to Your Head
The connection between your gut and brain isn’t just a vague notion; it’s a complex, bidirectional superhighway involving multiple communication channels. Understanding these pathways helps clarify how interventions like Intermittent Fasting, which primarily target the gut, can exert such significant influence over your ability to focus or cognitive function.
Meet the Vagus Nerve: The Direct Line
One of the most critical physical links is the vagus nerve, the longest cranial nerve, extending from the brain stem down to the abdomen and innervating major organs, including the gut [1, 3].
- Two-Way Traffic: The vagus nerve acts like a high-speed fiber optic cable, transmitting signals in both directions. Importantly, estimates suggest that 80-90% of the nerve fibers in the vagus nerve are afferent, meaning they carry information from the gut to the brain.
- Relaying Gut Status: It relays sensory information about gut distension, nutrient content, hormonal signals from the gut, and even signals generated by the gut microbiome to brain regions involved in mood, stress response, appetite, and potentially cognition [5]. Stimulating the vagus nerve (e.g., through deep breathing or even specific devices) is known to influence brain activity and mood.
Hormonal & Chemical Messengers: Crossing the Distance
Beyond direct nerve connections, the gut and brain communicate via chemical messengers circulating in the bloodstream:
- Gut Hormones: Cells lining the gut produce various hormones in response to food intake or fasting (e.g., ghrelin, leptin, PYY, GLP-1). These hormones travel through the blood and act on brain regions controlling appetite, satiety, and potentially energy metabolism relevant to focus.
- Microbiome Metabolites: As mentioned, gut microbes produce numerous metabolites, most notably Short-Chain Fatty Acids (SCFAs) like butyrate, propionate, and acetate, primarily by fermenting dietary fiber [2, 4]. SCFAs have profound effects:
- They serve as an energy source for gut lining cells, maintaining barrier integrity.
- They have anti-inflammatory properties systemically and potentially in the brain.
- They can influence neurotransmitter levels and even cross the blood-brain barrier or signal via pathways like the vagus nerve [4]. Changes in SCFA production due to dietary shifts or fasting can significantly impact brain function.
- Neurotransmitters: While gut-produced neurotransmitters like serotonin don’t easily cross the blood-brain barrier themselves, they influence local gut function and can signal the brain indirectly via the vagus nerve or by influencing immune cells [1].
The Immune System Connection: Inflammation as a Key Signal
The gut houses a huge portion of the immune system. The gut microbiome and the integrity of the gut barrier heavily influence immune activity.
- Leaky Gut and Inflammation: If the gut barrier becomes compromised (“leaky gut”), bacterial components (like lipopolysaccharide, LPS) can enter the bloodstream, triggering a systemic inflammatory response. This inflammation can reach the brain (neuroinflammation), contributing significantly to brain fog, fatigue, and impaired cognitive function [3, 5].
- Microbiome’s Role: The composition of the gut microbiome influences immune cell training and inflammatory signaling. Dysbiosis is often associated with increased gut permeability and inflammation.
This intricate network ensures constant communication. Disruptions anywhere along this gut-brain axis communication pathway – whether due to stress, poor diet, or gut dysbiosis – can negatively impact mental clarity. Conversely, strategies that promote gut health, like Intermittent Fasting, may foster clearer communication and sharper focus.
Fasting’s Gut Reset: Giving Your Second Brain a Break
Now we connect the dots. How does Intermittent Fasting leverage this intricate Gut-Brain Axis to potentially improve your focus? By giving your digestive system – your “second brain” – regular, scheduled downtime, IF initiates several changes that can positively influence gut health and, consequently, brain function.
Reducing the Digestive Workload: More Than Just Rest
Constantly eating means your gut is always working – secreting enzymes, contracting muscles, absorbing nutrients. This requires significant energy and blood flow diverted to the digestive tract.
- Energy Reallocation: Fasting periods allow this energy and blood flow to be potentially redirected elsewhere, like maybe even supporting cognitive processes.
- Reduced Exposure to Food Antigens/Irritants: Giving the gut lining a break from constant exposure to food components (some of which might be mildly inflammatory or irritating for certain individuals) can allow for rest and potential repair.
Potential Impact on Gut Lining Integrity (“Leaky Gut”)
The gut lining is a critical barrier. Chronic inflammation, poor diet, or stress can increase its permeability, allowing unwanted substances to leak into the bloodstream, triggering systemic inflammation that affects the brain [3].
- Fasting and Barrier Function: While research is ongoing and complex, some studies suggest that fasting periods might support gut barrier integrity [6]. This could be due to reduced inflammatory load, changes in microbial metabolites like butyrate (which fuels gut cells), or activation of repair processes like autophagy within the gut lining cells themselves.
- Less Inflammation = Clearer Head: By potentially reducing “leaky gut” and the resulting inflammatory signals traveling up the gut-brain axis, IF might contribute significantly to reducing neuroinflammation and alleviating brain fog.
Influencing Gut Motility: The “Housekeeping” Wave
During fasting periods, especially overnight, the gut engages in a specific pattern of contractions called the Migrating Motor Complex (MMC). This acts like a “housekeeping wave,” sweeping residual undigested material and bacteria down the digestive tract [1].
- MMC and Bacterial Overgrowth: Regular MMC activity helps prevent the overgrowth of bacteria in the small intestine (SIBO), a condition often linked to digestive issues and sometimes cognitive symptoms like brain fog.
- IF and MMC: Intermittent fasting naturally provides longer periods for the MMC to operate effectively between meals, potentially promoting a healthier distribution of gut microbes.
Shifting the Microbiome Landscape: Fasting’s Microbial Effect
Perhaps one of the most significant impacts of IF on the gut is its effect on the gut microbiome composition and function [2, 7].
- Nutrient Availability Changes: Fasting alters the fuel sources available to gut microbes. Different bacteria thrive on different nutrients. Regular fasting periods can shift the balance, potentially favoring bacteria that are more resilient or produce beneficial metabolites like SCFAs [4].
- Diversity and Function: Some studies suggest IF may influence microbial diversity (though results vary) and alter the functional output of the microbiome. For example, increased production of butyrate, known for its anti-inflammatory effects and role in gut health, has been observed in some fasting contexts [7].
- Microbial Rhythm: Just like us, gut microbes have daily rhythms. IF might help reinforce healthier microbial oscillations that are aligned with our own circadian rhythms.
By providing digestive rest, potentially improving barrier function, supporting gut motility, and influencing the microbiome, intermittent fasting sets the stage for a healthier gut environment, which is foundational for clearer communication along the gut-brain axis and ultimately, better focus.
From Gut Health to Head Space: Translating Changes into Focus
Okay, so Intermittent Fasting influences gut rest, barrier function, motility, and the microbiome. But how does all that gut-level activity actually translate into the sharper focus and mental clarity we’re aiming for? It comes back to the Gut-Brain Axis communication channels. A healthier gut sends healthier signals.
Calming the Inflammatory Storm: Less Noise, More Signal
As we discussed, a major way the gut impacts the brain is through inflammation. A leaky gut or an imbalanced microbiome can trigger low-grade systemic inflammation that readily translates into neuroinflammation [3, 5].
- IF’s Anti-inflammatory Gut Effect: By potentially improving gut barrier integrity and shifting the microbiome towards a less inflammatory state (perhaps increasing anti-inflammatory SCFA production [4, 7]), intermittent fasting can help turn down the volume on these inflammatory signals traveling to the brain.
- Reduced Neuroinflammation = Clearer Thinking: Neuroinflammation is strongly associated with brain fog, fatigue, slowed thinking, and difficulty concentrating. Reducing it creates a much better environment for optimal neuronal function and allows for clearer cognitive processing. Think of it as removing static from your brain’s radio signal.
Tuning Neurotransmitters and Brain Chemistry?
The gut microbiome doesn’t just influence inflammation; it actively participates in producing and modulating neurotransmitters or their precursors [1, 2].
- Microbes Making Mood Molecules: Gut bacteria can synthesize neurotransmitters like serotonin, GABA, and dopamine, or influence the availability of precursors like tryptophan (needed for serotonin). While these gut-produced neurotransmitters may not directly cross the blood-brain barrier in large amounts, they influence the ENS and can signal the brain via the vagus nerve [1].
- SCFAs and Brain Function: Short-chain fatty acids like butyrate, potentially increased by IF-induced microbial shifts, can influence brain function, potentially affecting neurotransmitter systems, promoting BDNF expression and having neuroprotective effects [4].
- The Focus Connection: By influencing the balance of key neurotransmitters involved in mood, attention, and reward, and potentially boosting factors like BDNF, the gut changes induced by IF could directly contribute to improved concentration and a more stable mental state conducive to focus.
Stabilizing Energy and Reducing Cognitive Load
A constantly working digestive system requires significant energy. An irritated or inflamed gut can also be an energy drain.
- Freeing Up Resources: Giving the gut regular breaks might free up metabolic resources that can be used by the brain.
- Reduced “Sickness Behavior”: Low-grade inflammation often triggers subtle “sickness behaviors,” including fatigue, reduced motivation, and brain fog [5]. By reducing the inflammatory load originating from the gut, IF might alleviate these focus-sapping symptoms.
Essentially, by fostering a healthier gut environment, Intermittent Fasting helps optimize the signals sent along the gut-brain axis. Less inflammatory noise, potentially better neurotransmitter balance, and reduced systemic drain all contribute to creating a brain state that is less foggy, more resilient, and better equipped for sustained focus and cognitive performance. It truly suggests that improving focus might start in your stomach.
Nourishing Your Gut-Brain Axis During Your Eating Window
Understanding the Gut-Brain Axis highlights that while Intermittent Fasting provides the crucial rest period, what you eat during your non-fasting eating window is equally vital for supporting both gut health and brain function. You can’t fast your way to focus if you’re constantly undermining your gut health when you do eat.
Feeding Your Friendly Microbes: The Power of Fiber
Your gut microbes, particularly the beneficial ones that produce those wonderful SCFAs, thrive on dietary fiber – specifically, prebiotic fiber found in plant foods that resist digestion in the small intestine [2, 4].
- Prebiotic Powerhouses: Include plenty of fiber-rich foods like:
- Vegetables (especially onions, garlic, leeks, asparagus, artichokes, leafy greens)
- Fruits (berries, apples, bananas – particularly slightly green ones for resistant starch)
- Legumes (beans, lentils, chickpeas)
- Whole Grains (oats, barley, quinoa)
- Nuts and Seeds (chia, flax, almonds)
- SCFA Production Boost: Providing ample fuel for your microbes encourages the production of butyrate and other SCFAs, supporting gut lining health, reducing inflammation, and positively signaling the brain [4, 7].
Polyphenols: Antioxidants for Gut and Brain
Polyphenols are compounds found in colorful plants that act as potent antioxidants and anti-inflammatories. They benefit both the gut and the brain directly, and also influence the microbiome [8].
- Sources: Berries, dark chocolate (in moderation), green tea, coffee, colorful vegetables, olive oil, herbs, and spices are rich in polyphenols. (See also “Top 10 Brain Boosting Foods“).
- Dual Action: They can directly combat oxidative stress in the gut and brain, and also act as prebiotics or modulate microbial composition, favoring beneficial species.
Fermented Foods: Probiotic Potential?
Fermented foods contain live bacteria (probiotics) that may temporarily colonize the gut and offer health benefits.
- Examples: Yogurt (plain, unsweetened with live cultures), kefir, sauerkraut, kimchi, miso, tempeh.
- Potential Benefits: While effects can be strain-specific and individual, regular consumption of diverse fermented foods may help support microbial diversity and gut function [2].
Healthy Fats: Supporting Both Ends
Healthy fats are crucial for brain structure and function (think omega-3s from fatty fish) but also play a role in gut health.
- Omega-3s: Found in fatty fish (salmon, mackerel), walnuts, flaxseeds, chia seeds. Have anti-inflammatory effects beneficial for both gut and brain.
- Monounsaturated Fats: Found in olive oil, avocados, nuts. Support overall cardiovascular health, which impacts brain blood flow, and contribute to a healthy inflammatory response.
Minimizing Gut Irritants
Just as important as adding beneficial foods is minimizing those that can harm gut health and trigger inflammation:
- Excess Sugar: Feeds less desirable microbes and promotes inflammation.
- Processed Foods: Often contain unhealthy fats, additives, and refined carbohydrates that negatively impact the microbiome and gut barrier.
- Artificial Sweeteners: Some research suggests potential negative impacts on gut microbes and glucose metabolism, though more study is needed.
- Excess Alcohol: Can irritate the gut lining and disrupt microbial balance.
By consciously choosing foods during your eating window that nourish your gut microbes, support barrier integrity, and reduce inflammation, you create a powerful synergy with your intermittent fasting practice, maximizing the positive communication along the gut-brain axis for optimal mental clarity.
Quick Takeaways: Gut-Brain Axis & Fasting for Focus
- Gut = “Second Brain”: Your gut has a complex nervous system (ENS) and trillions of microbes that profoundly influence your brain via the Gut-Brain Axis.
- Communication Superhighway: The gut and brain talk via nerves (vagus nerve), hormones, immune signals, and microbial metabolites (like SCFAs).
- IF Gives Gut Rest: Fasting provides digestive downtime, potentially supporting gut lining repair, promoting healthy gut motility (MMC), and reducing inflammatory load.
- Fasting Shifts Microbiome: IF alters nutrient availability for gut microbes, potentially shifting the balance towards beneficial bacteria and increasing anti-inflammatory SCFAs.
- Reduced Inflammation = Clearer Head: By improving gut health and reducing leaky gut, IF can lower systemic and neuroinflammation, a key contributor to brain fog.
- Neurotransmitter & BDNF Influence: Gut health and microbial metabolites can influence neurotransmitter balance and potentially boost BDNF, supporting mood and cognitive function.
- Eating Window Matters: Fuel your gut-brain axis during eating periods with fiber-rich foods (prebiotics), polyphenols (antioxidants), fermented foods (probiotics), and healthy fats. Minimize sugar and processed foods.
- Synergy for Focus: Combining the gut rest from IF with gut-supportive nutrition during eating windows optimizes Gut-Brain Axis communication for enhanced mental clarity and focus.
Conclusion
The quest for enhanced focus often leads us down paths exploring brain hacks, productivity techniques, or specific nutrients. Yet, as we’ve journeyed through the intricate connections of the Gut-Brain Axis, it becomes compellingly clear that the state of our digestive system plays a profoundly underestimated role in our cognitive performance. The concept of a “second brain” in our gut, teeming with microbes and communicating constantly with our primary brain, shifts our perspective. Improving focus isn’t just about what happens from the neck up; it truly might start in your stomach.
Intermittent Fasting emerges as a powerful modulator of this crucial axis. By providing regular periods of digestive rest, IF allows the gut environment to reset and potentially repair. It influences the composition and function of the vital gut microbiome, potentially favoring beneficial microbes and the production of anti-inflammatory compounds like SCFAs [4, 7]. It may help strengthen the gut barrier, reducing the “leakiness” that contributes to systemic and neuroinflammation – a known culprit behind brain fog [3, 6]. These gut-level changes translate into altered signals sent via nerves, hormones, and the immune system, ultimately creating a brain environment more conducive to clear thinking and sustained concentration.
However, fasting is only half the equation. The real magic happens when the restorative periods of IF are combined with conscious, gut-supportive nutrition during the eating window. Feeding your beneficial microbes with fiber, providing antioxidants through polyphenols, and including healthy fats creates a synergistic effect, optimizing the Gut-Brain Axis for peak performance.
So, the next time you’re considering strategies to sharpen your mind, don’t forget to “trust your gut” – literally. By leveraging Intermittent Fasting to support your digestive health and making smart food choices, you’re not just managing your weight or metabolism; you’re actively tending to the foundational communication network that underpins your cognitive function. A happy gut truly can contribute to a happier, more focused brain.
Gut Feelings on Focus? Share Your Experience!
Has learning about the Gut-Brain Axis changed how you view Intermittent Fasting or your diet?
- Have you noticed changes in digestion alongside changes in mental clarity when practicing IF?
- Do you focus on specific gut-healthy foods during your eating window?
- Any personal experiences linking gut health improvements (or issues) to your ability to focus?
We’d love to hear your thoughts and experiences in the comments below!
If you found this exploration of the gut-brain connection insightful, please share it with others interested in the deeper mechanisms behind IF and focus!
Gut-Brain Axis FAQs: Your Questions Answered
- How quickly can Intermittent Fasting improve gut health enough to affect focus?
- Changes in the gut microbiome can occur relatively quickly, within days of dietary shifts like starting IF [7]. However, translating these changes into noticeable improvements in gut barrier function, inflammation, and ultimately focus, likely takes longer – potentially several weeks of consistent practice combined with a supportive diet during the eating window.
- Can IF actually worsen gut issues or brain fog for some people?
- While generally beneficial, IF could potentially exacerbate issues for some individuals, especially initially or if done improperly. Starting too aggressively, poor food choices during the eating window, underlying gut conditions (like SIBO, if MMC isn’t sufficient), or inadequate hydration/electrolytes could lead to digestive upset or worsening brain fog. Gradual adaptation and listening to your body are key. Consult a healthcare provider if issues persist.
- Do I need to take probiotics while doing Intermittent Fasting for gut-brain benefits?
- Probiotics aren’t strictly necessary. Focusing on prebiotic fiber during your eating window to feed your existing beneficial microbes is often more impactful [2, 4]. Including naturally fermented foods provides some probiotics. If considering supplements, consult a professional, as effects are strain-specific and not guaranteed.
- Is the vagus nerve the main way fasting affects the brain via the gut?
- The vagus nerve is a major pathway, transmitting signals about the gut environment (including microbial activity) directly to the brain [1, 3]. However, it’s not the only way. Hormonal changes, circulating microbial metabolites like SCFAs, and modulation of the immune system/inflammation are also crucial components of the gut-brain axis communication influenced by fasting.
- If I improve my gut health through diet alone, will I get the same focus benefits as using IF?
- Improving gut health through a whole-foods, high-fiber diet is definitely beneficial for the gut-brain axis and can improve focus. However, Intermittent Fasting adds the unique element of prolonged digestive rest, which triggers specific processes like enhanced autophagy in gut cells and potentially more significant shifts in gut microbiome rhythm and function [6, 7]. Combining both approaches likely offers synergistic benefits for cognitive function.
References
- Furness, J. B., Callaghan, B. P., Rivera, L. R., & Cho, H. J. (2014). The enteric nervous system and gastrointestinal innervation: integrated local and central control. Advances in experimental medicine and biology, 817.
- Rinninella, E., Raoul, P., Cintoni, M., Franceschi, F., Miggiano, G. A. D., Gasbarrini, A., & Mele, C. (2019). What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms, 7(1).
- Bonaz, B., Bazin, T., & Pellissier, S. (2018). The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Frontiers in neuroscience, 12.
- Silva, Y. P., Bernardi, A., & Frozza, R. L. (2020). The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Frontiers in endocrinology, 11.
- Martin, C. R., Osadchiy, V., Kalani, A., & Mayer, E. A. (2018). The Brain-Gut-Microbiome Axis. Cellular and molecular gastroenterology and hepatology, 6(2).
- Patterson, R. E., & Sears, D. D. (2017). Metabolic Effects of Intermittent Fasting. Annual review of nutrition, 37.
- Liu, Z., Dai, X., Zhang, H., Shi, R., Hui, Y., Jin, X., … & Liu, H. (2020). Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Nature Communications, 11(1).
- Williamson, G. (2017). The role of polyphenols in modern nutrition. Nutrition bulletin, 42(3).